Joe Biden Drives Stake Through Heart Of Surprise Medical Billing
Quick! Nuke the site from orbit, just to be sure!
The Biden administration issued an interim rule aimed at ending the evil ugly practice of surprise medical billing Thursday, following up on a law passed by Congress back in December. The new rule, released by the departments of Health and Human Services (HHS), Treasury, and Labor, will go into effect on January 1, 2022, and should largely eliminate surprise medical billing, at least for people with health insurance through their employers, or who buy individual plans on the private market.
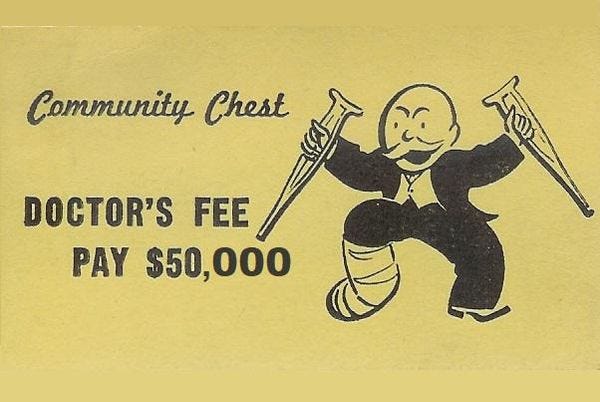
So what the hell is surprise medical billing? It occurs when somebody uses medical services that would be covered by their insurance, but which involves some part of service that — surprise! — is actually out of network, and billed at an insanely high rate. For instance, someone might make sure their planned surgery is done at an in-network hospital, by an in-network surgeon, but — surprise! — the anesthesiologist that day is out of network, and the patient is billed for tens of thousands of dollars. This practice has gotten much much worse as private equity firms have taken over American healthcare, because the whole point is to extract as much money as possible from patients, fairness be damned. Cory Doctorow has an excellent Twitter thread on how it all works, go read it, you.
As part of last year's big omnibus budget bill, Congress passed the "No Surprises Act," which authorized HHS to enact rules to put the kibosh on surprise medical billing. The resulting 411-page rule still needs to go through a routine 60-day public comment period and other administrative steps, but it's not likely to be modified much, because public support for reining in the practice is so strong. Let's take a look at how this sucker will work!
Fierce Healthcare has the skinny . The rule will
ban any surprise billing for emergency services regardless of where they are provided, including if they are air medical services. Such services must be treated via an in-network basis.
Other provisions of the rule include banning out-of-network charges without advance notice, out-of-network charges for ancillary care and any out-of-network charge for cost-sharing for emergency and nonemergency services.
"Patient cost-sharing, such as co-insurance or a deductible,cannot be higher than if such services were provided by an in-network doctor, and any coinsurance or deductible must be based on in-network provider rates," according to a release from HHS.
The rule would also forbid insurance plans from requiring prior authorization for emergency services, regardless of whether the policyholder goes to a hospital that's in network or not, or whether the providers of the emergency services are in or out of network.
So if suddenly you are run over by a truck , you will no longer be expected to emerge from your concussed state and tell the EMTs to take you to an in-network hospital, or to call your health insurer's call center to authorize treatment before they sew your leg back on. And even if an assistant surgeon scrubs in, you can't be billed more than the co-pay you'd have to pay for in-network treatment.
The rules will also limit how much can be charged for air ambulance services in emergencies, another huge source of surprise billing.
Again, this is a hell of a big change, and will reduce one of the biggest drivers of medical costs in our god damned for-profit medical system. The Wall Street Journal explains just how big a problem it is:
Out-of-network charges have added to medical debt and rising out-of-pocket payments for consumers: An April 2021 study in the journal Health Affairs found that patients receiving a surprise out-of-network bill for emergency physician care paid more than 10 times as much as in-network emergency patients paid out-of-pocket. [...]
Out-of-network charges from anesthesiologists, pathologists, radiologists and assistant surgeons increase spending by $40 billion annually, according to researchers at the Yale School of Public Health.
Additional rules are still in the offing, particularly when it comes to settling disputes between providers and insurers over who pays how much when there's a dispute. That's going to be contentious, because there's a lot of money at stake. The big thing is that the Biden administration seems determined that, going forward, patients won't be the ones getting soaked.
We still need huge reforms, like some kind of single-payer system that incorporates cost controls, as you'd find in Europe. But this is a huge change for the better.
[ Cory Doctorow on Twitter / Fierce Healthcare / Naked Capitalism ]
Yr Wonkette is funded entirely by donations from readers like you, but we like YOU best, never forget it. If you can, please share some love with us, won't you? And by love we mean money, comrade.
Do your Amazon shopping through this link, because reasons .



when they are telling me what I can prescribe, they are practicing medicine
Now if they would just do something about hospitals that double-bill and send patients to collection agencies, especially those they've already double-billed (looking at YOU, UVA Medical Systems!!!!). Those never get exposed unless local papers do the exposing. Thanks to the Roanoke papers, UVA at least did, but I'm still mad at them and won't go there.